The importance of artificial intelligence (AI) in clinical settings has grown significantly, sparking discussions on best practice for AI governance structures and identifying key stakeholders in building a long-lasting AI strategy. Specifically, radiologists have been at the forefront of embracing AI, acknowledging the potential it holds to transform their workflows, such as reducing reading times and reprioritizing worklists.
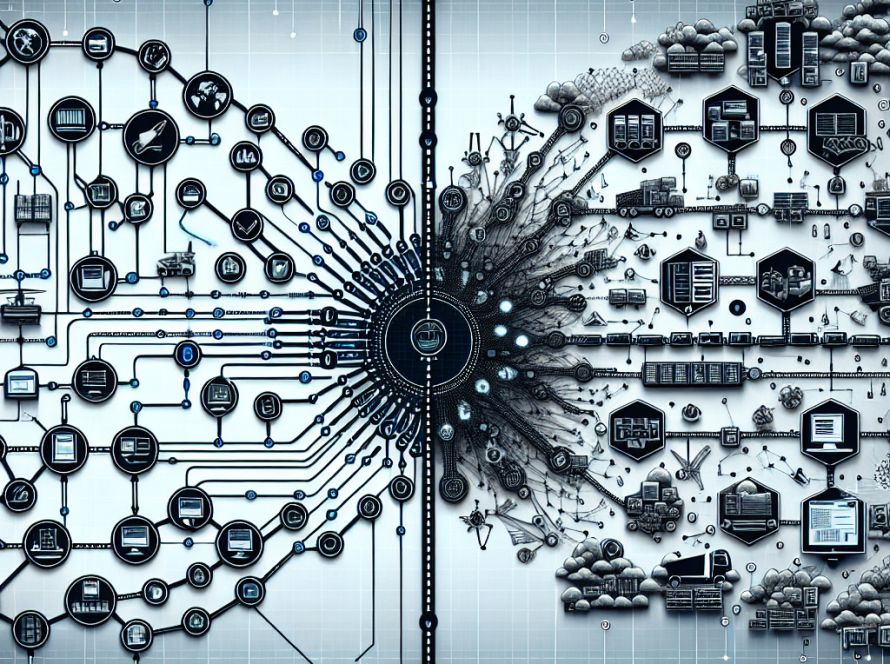
Three key areas need to be considered for a sustainable AI strategy in the radiology department. Firstly, recognizing and leveraging the potential of AI across the broader healthcare enterprise is crucial. While AI algorithms have proven successful in addressing specific use cases, the long-term stability and scalability of these solutions must be assessed. Adding a new algorithm from a different vendor, for instance, could create unforeseen complications. It is therefore important for radiology leaders to deliberate on the integration of different algorithms and potential conflicts arising from such arrangements.
A hypothetical example to illustrate this point could be an emergency department (ED) patient coming in following a car accident. The patient undergoes a chest and abdomen CT scan. AI algorithms would then be selected to analyze each scan. This translates to configuring the system to ‘decide’ which algorithms to use for each exam, operating as an added layer of intelligence always in the background. Running multiple algorithms concurrently allows the identification of both expected and unexpected pathologies.
The second consideration involves the experience of the radiologist. In a scenario where a health system has 20 different AI algorithms, questions about the status of each algorithm, handling urgent acute findings, as well as incorporating AI results into reports, all need to be addressed. A well-structured AI platform should seamlessly present the AI status and results in an accessible, intuitive interface.
Lastly, for an enterprise-wide AI platform, the ability to apply various algorithms based on the scan type and anatomy present in an image is critical. This approach not only identifies the expected issues related to the patient’s condition but also unexpected findings, leading to improved patient outcomes.
Looking ahead, as the AI industry is projected to consolidate, healthcare systems need to be discerning when choosing potential AI partners to ensure long-lasting clinical and financial returns on the investment in AI technology. Key requirements include data normalization, single interfaces and streamlined workflow integrations to provide a single point of contact. Therefore, radiology departments need to be on the frontline advocating for robust AI platforms.